Abstract
Transfusion-dependent non-severe aplastic anemia (TD-NSAA) refers to aplastic anemia (AA) that is dependent on blood transfusion but does not fulfilling the criteria for severe AA (SAA). It has been clear that allogeneic hematopoietic stem cell transplantation (HSCT) and anti-thymocyte globulin (ATG)-based immunosuppressive therapy (IST) is the front line for the treatment of SAA, but there is no consensus on the treatment timing and strategy for TD-NSAA. The natural history observation reported that the progress-free survival (PFS) of TD-NSAA at 60 months after diagnosis is around 62%, but decreased significantly to 22% at 120 months. In China, the practical guideline recommends cyclosporine-based IST with or without hematopoietic stimulating regimes (such as androgens) as initial treatment, and further treated as SAA if no response was observed after 6 months management. As reported, the hematopoietic response of ATG-based IST was much better than CsA-based IST (75% Vs. 55.8%, 6-month) for TD-NSAA, however, the relapse and clonal expansion are still the unavoidable events. For HSCT, the long-term PFS is much better than IST for SAA, but the complications (including graft versus host disease, various infection, etc.), transplantation related mortality, as well as donor availability still limited its application. At present, there is limited data compared the efficiency of HSCT and IST for TD-NSAA. With the development of haplo-identical transplantation in China, most TD-NSAA own a donor, and we also performed HSCT for those young patients after informed consent. Herein, we respectively compared the efficiency of ATG-based IST and HSCT for TD-NSAA, and also analyzed the risk factors that contribute to the overall survival (OS) as well as event free survival (EFS).
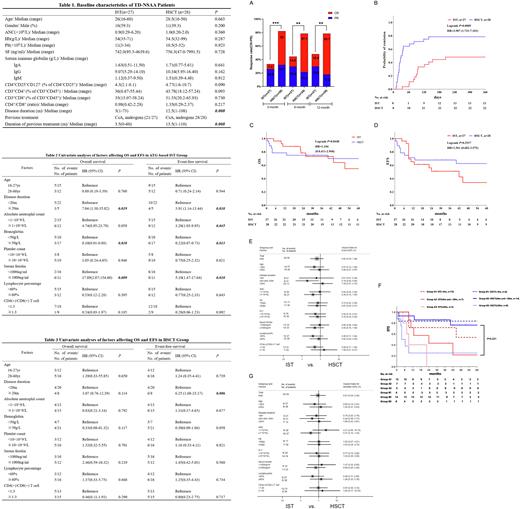
During Jul 2011 to Dec 2019, 97 TD-NSAA patients were diagnosed in our cohort, among them, 5 only received supportive treatment, 30 received CsA-based IST with or without androgen, and the other 62 patients received HSCT or ATG-based IST therapy. We further analyzed the efficiency and prognosis of 55 patients aged 16-60 years old who received HSCT or ATG-based IST therapy. Among them, 27 (49.09%) patients received ATG-based IST, and the others performed HSCT (including 14 from sibling donor, 7 from haplo-identical donor and 7 from unrelated donor) (the baseline information showed in Table1). Results showed that the 12-month overall response rate (ORR) of ATG-based IST and HSCT were 48.1% (with 18.52% CR) and 78.57% (with 60.71% CR), respectively (P=0.04, Fig A). The median time of achieving transfusion-free was 94(35-205) and 24(11-139) days, respectively in ATG-based IST and HSCT group (P<0.001, Fig B). The 5-year OS and EFS rates were 54.9±13.3% and 34.5±12.1% in ATG-based IST group respectively, and 70.0±9.0% and 62.6±9.6% in HSCT group, while no statistically differences was observed (Fig C and D). To explore the possible influencing factors of 5-year OS and EFS, we performed COX regression analysis based on age, disease duration, baseline absolute neutrophil count (ANC), hemoglobin (HB), platelet count (PLT), serum ferritin (SF), lymphocyte percentage, and CD4/CD8 ratio. Univariate analysis showed that disease duration, baseline HB, SF, and ANC may affect OS and EFS of patients in ATG-based IST group (Table 2), and multivariate analysis showed that SF≧1000ng/ml was an independent risk factor for OS in ATG-based IST group. While in the HSCT group, patients with disease duration≧20 months had a higher risk of events (Table 3). The subgroup analysis showed that in HSCT group, patients with disease duration of 6 to 20 months had a lower risk of events (HR=0.196, 95%CI: 0.046-0.832); the HR of the group <6 months and ≥20 months were not statistically significant (Fig E). TD-NSAA patients with disease duration between 6 months and 20 months had a higher EFS rate in HSCT group than that in ATG-based IST group (Fig F). The subgroup analysis of mortality was not statistically significant (Fig G).
To conclusion, TD-NSAA patients should be actively treated, patients with shorter disease duration and no iron overload may achieve a better response. The 12-month ORR in the HSCT group was higher than that in the IST group, but there was no significant difference in OS rate and EFS rate, even there is a great difference tendency. For TD-NSAA patients with a disease duration between 6 to 20 months, HSCT has a higher EFS rate than IST, which may be a better choice.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal